Introduction
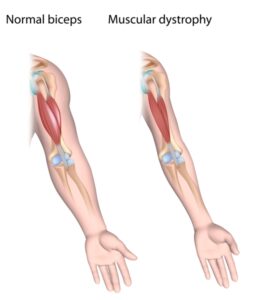
Muscular Dystrophy (MD) refers to a group of genetic disorders that cause progressive muscle weakness and degeneration. It affects the muscles responsible for movement, leading to difficulties in mobility and everyday activities. Muscular Dystrophy can vary in its severity, age of onset, and progression rate, but it often requires ongoing management and support.
Symptoms
The symptoms of Muscular Dystrophy can vary depending on the specific type of the condition and the muscles affected. Common symptoms include muscle weakness, muscle wasting, difficulties with coordination and balance, limited range of motion, and, in some cases, contractures (joint stiffness). The progression of symptoms can be gradual, and they may affect both voluntary and involuntary muscles, such as those involved in breathing and swallowing.
Diagnosis
Diagnosing Muscular Dystrophy typically involves a combination of medical history, physical examination, and diagnostic tests. Healthcare professionals, such as neurologists, may conduct muscle strength and function assessments, genetic testing to identify specific gene mutations associated with MD, and electromyography (EMG) to measure the electrical activity of muscles. These diagnostic tools help determine the specific type of Muscular Dystrophy and guide appropriate treatment and management.
Treatment
While there is currently no cure for Muscular Dystrophy, treatment aims to manage symptoms, slow the progression of the disease, and improve quality of life. Treatment plans are tailored to the specific needs of each individual and may include a combination of interventions. These can include physical therapy to improve strength, mobility, and flexibility, occupational therapy to aid in activities of daily living, and assistive devices like braces, wheelchairs, or mobility aids to enhance independence and mobility. Medications, such as corticosteroids, may be prescribed to help manage symptoms and delay muscle degeneration. In some cases, surgical interventions or respiratory support may also be necessary.
Lifestyle Changes
Living with Muscular Dystrophy often requires certain lifestyle adjustments:
Conserving Energy: Managing fatigue is important, as individuals with MD may have reduced muscle strength and endurance. Pacing activities, taking breaks, and balancing rest with appropriate physical activity can help conserve energy and prevent overexertion.
Accessibility and Assistive Devices: Modifying the living environment to improve accessibility, such as installing ramps or handrails, can facilitate mobility. Using assistive devices like braces, walkers, or specialized tools can aid in daily tasks and enhance independence.
Emotional Support: Muscular Dystrophy can have emotional and psychological impacts. Seeking support from loved ones, joining support groups, or engaging in counseling can provide valuable emotional support and coping strategies.
Regular Monitoring and Healthcare: Regular check-ups with healthcare professionals are important to monitor the progression of the disease, address any new concerns, and adjust treatment plans accordingly. Staying informed and actively participating in healthcare decisions is crucial.
Adaptive Strategies: Exploring adaptive strategies and technologies, such as assistive communication devices or home modifications, can help individuals with Muscular Dystrophy overcome challenges and maintain an active lifestyle.
Living with Muscular Dystrophy may present unique challenges, but with proper support, medical care, and lifestyle adjustments, individuals can lead fulfilling lives. It is essential to focus on abilities, set realistic goals, and seek opportunities for social engagement and personal growth. With resilience, self-care, and a supportive network, individuals with Muscular Dystrophy can navigate their journey with strength and determination.







